People who are overweight or obese are at higher risk for at least 13 different types of cancer, which together make up about 40 percent of all cancer diagnoses in the United States, according to the latest Vital Signs report from the Centers for Disease Control and Prevention (CDC). Only smoking is a bigger cancer risk factor.
While new cancer diagnoses have decreased overall since the 1990s, increases in obesity-related cancers are likely slowing this progress, according to the CDC. About two thirds of U.S. adults and nearly a third of children are considered to be either overweight (body mass index, or BMI, of 25.0 to 29.9) or obese (BMI of 30.0 or higher).
“A majority of American adults weigh more than recommended—and being overweight or obese puts people at higher risk for a number of cancers—so these findings are a cause for concern,” CDC director Brenda Fitzgerald, MD, said in a CDC press release. “By getting to and keeping a healthy weight, we all can play a role in cancer prevention.”
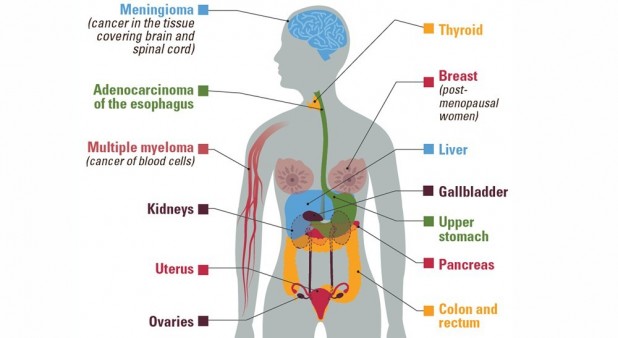
The Vital Signs report is based on an analysis by CDC and National Cancer Institute researchers of 2014 data from the United States Cancer Statistics database. The study, recently published in the CDC’s Morbidity and Mortality Weekly Report, focused on 13 cancers that the International Agency for Research on Cancer has linked to being overweight or obese:
- Breast cancer in postmenopausal women
- Colon and rectal cancer
- Esophagus cancer (adenocarcinoma)
- Gallbladder cancer
- Kidney Cancer
- Liver cancer
- Meningioma (cancer of the membranes covering the brain)
- Multiple myeloma
- Ovarian cancer
- Pancreas cancer
- Stomach cancer
- Thyroid cancer
- Uterine cancer
More than 631,000 people in the United States were diagnosed with obesity-related cancers in 2014, according to the report. Together, these cancer types account for about 40 percent of the nearly 1.6 million cancers diagnosed annually—55 percent of all cancers diagnosed in women and 24 percent of those diagnosed in men.
Two thirds of obesity-related cancer cases occur in people between ages 50 and 74. Women have about twice the rate of obesity-related cancer as men (218 versus 115 per 100,000 people), largely attributable to breast, ovarian and endometrial uterine cancer. Cancers common in men, including lung and prostate cancer, do not appear to be obesity-related.
Obesity-related cancers, excluding colorectal cancer, increased by 7 percent between 2004 and 2015 (from 123 to 132 cases per 100,000 people), even as other types of cancer fell by 13 percent (from 306 to 267 cases per 100,000). Colon cancer, however, declined by 23 percent (from 50 to 38 cases per 100,000) during this period. Colon cancer was considered separately because precancerous changes can be detected with regular screenings and treated before they become cancerous.
Studies show that obese people are about 30 percent more likely to develop colorectal cancer than people with a healthy weight, and overweight or obese women are two to four times more likely to develop endometrial cancer than women with a healthy weight, according to the study authors. Even an 11-pound weight gain since early adulthood is associated with increased risk for obesity-related cancers.
These findings add to the growing body of evidence showing that a balanced diet, exercise and maintaining a healthy weight can help prevent cancer. An overall healthy diet is more beneficial than eating or avoiding specific foods. The link between cancer and obesity is not fully understood, but chronic inflammation and altered hormone levels appear to play a role.
“As an oncologist, when people ask me if there’s a cure for cancer, I say, ‘Yes, good health is the best prescription for preventing chronic diseases, including cancer,’” said Lisa Richardson, MD, director of the CDC’s Division of Cancer Prevention and Control.
The Vital Signs report and a related commentary in the Journal of the American Medical Association discuss some steps that individuals, health care providers and communities can take to promote healthy weight and reduce the risk of obesity-related cancers.
- Individuals can follow healthy diet guidelines and do at least 150 minutes of moderate intensity physical activity each week.
- Health care providers can measure patients’ weight and BMI, counsel them about maintaining a healthy weight and refer obese patients to programs to help them lose weight.
- Communities can make it easier for residents to choose healthy food options (for example by increasing access to farmers’ markets) and make it safer to be physically active (for example by creating walking trails and bike lanes).
- Schools can offer healthy food options, support quality physical education and encourage students to walk or bike to school.
- Workplaces can offer health food in cafeterias and vending machines and encourage physical activity.
- Families can participate in physical activities together and limit screen time in front of TVs and computers.
“Achieving sustainable weight loss requires comprehensive strategies that support patients’ efforts to make significant lifestyle changes,” Greta Massetti, PhD, of the CDC’s Division of Cancer Prevention and Control and coauthors wrote in their JAMA commentary. “Linking community obesity prevention, weight management and physical activity programs with clinical services can connect people to valuable prevention and intervention resources in the communities where they live, work and play. Such linkages can give individuals the encouragement they need for the lifestyle changes that maintain or improve their health.”
Click here to read the complete Vital Signs report.
Click here to see a CDC infographic about cancer and obesity.






Comments
Comments